833 HOSPITAL PRESUMPTIVE ELIGIBILITY
Hospital Presumptive Eligibility is a requirement of the Affordable Care Act (ACA) that was effective January 1, 2014. States are required to allow approved hospitals to presumptively determine eligibility for certain categories of MAGI Medicaid and Breast & Cervical Cancer Medicaid (BCCM / Ladies First / AK B+C).
HPE can only be used for the following MAGI Medicaid categories:
1) Children Under Age 19;
2) Parents/Caretaker Relatives;
3) Pregnant Women;
4) Former Foster Care;
5) Expansion Group; and
6) Breast and Cervical Cancer / Ladies First (see ADLTC section 575)
Simplified Determinations
Hospitals will use a simplified application (HPE 1) as states are not allowed to ask all of the questions that are listed on the full Medicaid application. Hospital Presumptive Eligibility is only temporary coverage. In order to receive ongoing Medicaid coverage, these individuals must submit a regular Medicaid application and be found eligible for Medicaid by the Division of Public Assistance. DPA is authorizing the Medicaid benefits based on the hospital's determination.
The Required Gen 50C
Hospitals will assist individuals that have been approved for Hospital Presumptive Eligibility to complete a paper Gen 50C for Medicaid and submit it to their local DPA office within the approved HPE period. Individuals approved for full MAGI Medicaid will be authorized in ARIES, if possible.
The presumptive eligibility period begins the date that the hospital determines the applicant presumptively eligible for Medicaid and ends the earlier of:
1) The date the ineligibility determination for regular MAGI Medicaid is made, if a full application for MAGI Medicaid is filed by the end of the month after the month that presumptive eligibility is determined; or
2) The last day of the month after the month of the HPE Medicaid determination, if a full application for Medicaid is not filed by that date.
Variable End Date
The end date for the Hospital Presumptive Eligibility depends on whether or not the individual submits a full Medicaid application during the approved HPE coverage period. If an individual received Medicaid through HPE and a full Medicaid application is received within the HPE coverage period, the application must be prioritized and processed immediately to ensure the HPE period is adjusted as necessary. The local office receiving the full Medicaid application must make sure that the Hospital Presumptive Eligibility ends when it should, which could mean extending or shortening the HPE approved period.
Example:
A GEN 50C is received on 10/21 for Medicaid. The individuals listed on the Gen 50C are looked up in EIS to see if they received Medicaid under FSO 15. It is found that the individual was authorized HPE Medicaid from 09/15 through 10/31. This Medicaid application needs to be prioritized and processed immediately. This is to ensure that a Medicaid determination (approval or denial) on the regular Medicaid application is made before the authorized HPE Medicaid ends. If a Medicaid eligibility determination is not made by 10/31, the HPE Medicaid case must be processed and authorized for another month (this will also require reopening the HPE Medicaid case). If DPA determines that this individual is ineligible for Medicaid on 10/22, the previously authorized HPE period will need to be shortened.
DPA will only alter (shorten or extend) the HPE benefit if the individual submits a full Medicaid application within the approved HPE period. Applications received prior to or after the HPE period will not affect the HPE benefits start, and end date authorized by the hospital.
The Approved Hospital List
Please refer to the "Approved Hospital List" prior to authorizing hospital presumptive Medicaid. This document includes:
If an HPE packet is received from a hospital that is not on the approved list or the Presumptive Eligibility Worksheet (HPE 2) is signed by a hospital staff member not on the approved list, do not approve the HPE benefit until you verify eligibility by contacting policy at hss.dpa.policy@alaska.gov.
Note:
There are two approved groups making HPE determinations at Alaska Native Medical Center: Alaska Native Tribal Health Consortium and Southcentral Foundation. Make sure you are using the correct caseload id and faxing the coupon to the correct group.
How the HPE Application Affects Ongoing Benefits
Information entered by the applicant on the HPE application (HPE 1) is information reported to the hospital in order for them to make an eligibility determination. The information is not considered to be a report of change to DPA. We should not use the information showing on the HPE application to make case changes to any open program the client may be receiving. Only if the client applies for regular Medicaid using a full Medicaid application should we check for report of change.
The Hospital HPE Screening
The hospital staff member must screen the applicant for HPE eligibility. This screening involves the applicant or their spouse attesting to the Medicaid eligibility factors required for HPE. An authorized representative can sign the HPE application if the applicant is unable to do so but the applicant or their spouse must verbally answer the HPE screening questions. If the applicant is unable to do so, hospitals have been instructed not to authorize HPE benefits. A GEN 50C should be submitted to their local DPA office for a full Medicaid determination.
An individual can only have one hospital presumptive eligibility approval within a 12-month period, starting with the month of the initial HPE period. A pregnant woman can be found presumptively eligible once per pregnancy, even if the pregnancies occur within the same 12-month period.
Example 1:
An individual received HPE benefits on 9/8/15. The 12-month period for this client is 9/2015 – 8/2016 so the client is eligible for HPE benefits again 9/1/2016.
Example 2:
A pregnant woman received HPE coverage starting 09/08/2015. The pregnancy ended, and she becomes pregnant again on 07/02/2016. As it is a second pregnancy, she is eligible for another HPE period, even though it has not been a year since the initial HPE period.
Example 3:
A woman received HPE coverage for Expansion Medicaid starting 09/08/2015. She becomes pregnant and applies for HPE coverage on 01/05/2016. As the initial HPE period was not for Pregnant Woman Medicaid and it has not been 12 months since the approval, she is not eligible for HPE coverage from the 01/05/2016 application.
A qualified hospital is one that participates as a provider under the Medicaid state plan and has notified the Medicaid agency of its election to make presumptive eligibility determinations and agrees to make presumptive eligibility determinations consistent with state policies and procedures. A qualified hospital must help individuals complete a full Medicaid application.
If any approval paperwork is received from a hospital not on this list or the hospital presumptive eligibility determination is signed by a hospital worker not listed, please contact the Policy & Program Development Team at hss.dpa.policy@alaska.gov.
Each hospital that would like to make presumptive eligibility determinations must indicate their interest by completing a Memorandum of Understanding (MOU) with the Division of Public Assistance. Interested hospitals that do not already have a HPE MOU in place should send their request for a MOU to hss.dpa.policy@alaska.gov
HPE Training for Hospital Staff Members
Once an HPE MOU has been approved for the hospital, every hospital worker that will make these determinations must complete on-line HPE training created by SD&T and pass a knowledge test prior to any determinations being made.
A list of all approved hospitals and hospital workers that have successfully completed training is available on the DPAweb under the MAGI Medicaid manual at http://dpaweb.hss.state.ak.us/node/15.
Client Attestation
Hospitals are not allowed to verify information provided by an HPE applicant. They will take client attestation of specific eligibility factors. If the individual(s) are found eligible for HPE benefits, the hospital will fax the initial HPE packet to DOST for processing. If any of these initial HPE application materials are accidentally sent directly from the hospital to a local DPA office for processing, please send them to hss.dpadost@alaska.gov immediately.
The existing information in EIS should not be changed based on a HPE application, with one exception: if the individual does not currently receive public assistance benefits and the only change is a slight name difference (Ex: Daniel VS Danny). Remember to create an alias if making a "given" name change. A HPE application is not a report of change to DPA.
Duplicating Medicaid Benefits
If the individual is found to be eligible for regular Medicaid, there is no need to make any changes to the HPE case in EIS, as this should already be closed. When making the Medicaid eligibility determination in ARIES, the Medicaid should start the first day of the month that the application was filed, and we determine that the household is eligible. Retroactive Medicaid requests should be handled normally.
Changing (Pulling Back) HPE End Date(s)
When a HPE recipient submits a GEN 50C MAGI Medicaid application prior to the end of their HPE period and the client is determined ineligible for MAGI Medicaid, the HPE END DATE must be updated on the HPE case and pulled-back to the date that MAGI Medicaid ineligibility was determined. This includes if you must deny the Medicaid application because the household did not provide the verification necessary to make an eligibility determination.
Example:
Jon was approved for HPE benefits from 03/13/18 - 04/30/18. Jon submitted a GEN 50C to his local office on 04/27/18. Since the application was submitted within the approved HPE period, it was processed immediately. The application was pended for verification needed to make an eligibility determination that was not due until 05/08/18. HPE benefits for Jon must be issued for 05/18 since we are unable to make an eligibility determination by 04/30/18. Jon fails to provide the verification, and his Medicaid application is denied on 05/11/18. The HPE benefits must be ended on 05/11/18, the date the Medicaid application is denied.
Newborns
Newborns born to women during the HPE period are not eligible for newborn "BA" Medicaid as they were not born to women eligible for and receiving Medicaid in the month of delivery.
Exception:
If regular retroactive Medicaid was approved for the mother in the birth month, the newborn would then be eligible for newborn "BA" Medicaid.
Example:
Providence Hospital determines Sue Johnson presumptively eligible for Medicaid on 09/08/17 in the pregnant woman category and provides Sue with an approval letter. Sue's eligibility for HPE Medicaid ends on 10/31/17. However, since Sue applied for full Medicaid in the month she gave birth and we issued Medicaid starting 10/01/17 to cover the birth expenses, the baby is also eligible for "BA" Medicaid.
Requests for Retroactive Medicaid Coverage
If the applicant submits a regular application and requests Retroactive Medicaid coverage, the same rules for retroactive coverage apply. Retroactive months are the 3 months immediately preceding the submission of a regular Medicaid application.
A state may disqualify a hospital from conducting presumptive eligibility determinations if the state finds that the hospital is not making or is not capable of making accurate presumptive eligibility determinations in accordance with applicable state policies and procedures.
Individuals determined eligible under hospital presumptive eligibility are provided the same coverage as those provided under the eligibility group for which hospital presumptive eligibility is determined.
The exception is pregnant women whose coverage is limited under hospital presumptive eligibility and does not cover inpatient hospitalization, including labor and delivery. If the woman is approved for regular pregnancy Medicaid after completion of a Gen 50C, coverage will include these inpatient services.
Questions regarding covered services should be directed to the Alaska Medicaid Recipient Helpline at 800-780-9972.
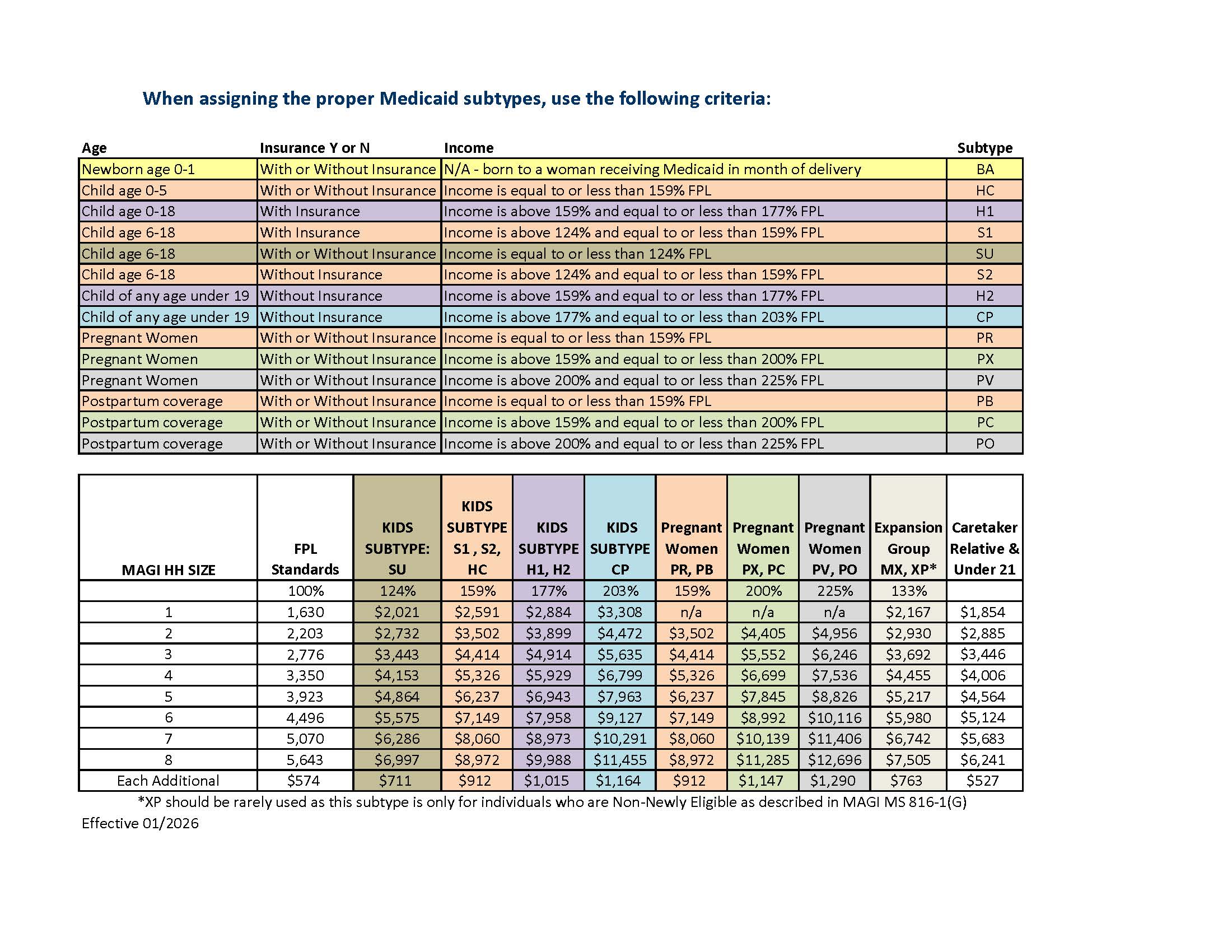
The income standards for all MAGI Medicaid categories based on the FPL are revised each April. The Parent/Caretaker Relative and Under 21 categories are based on the COLA and are revised each January.
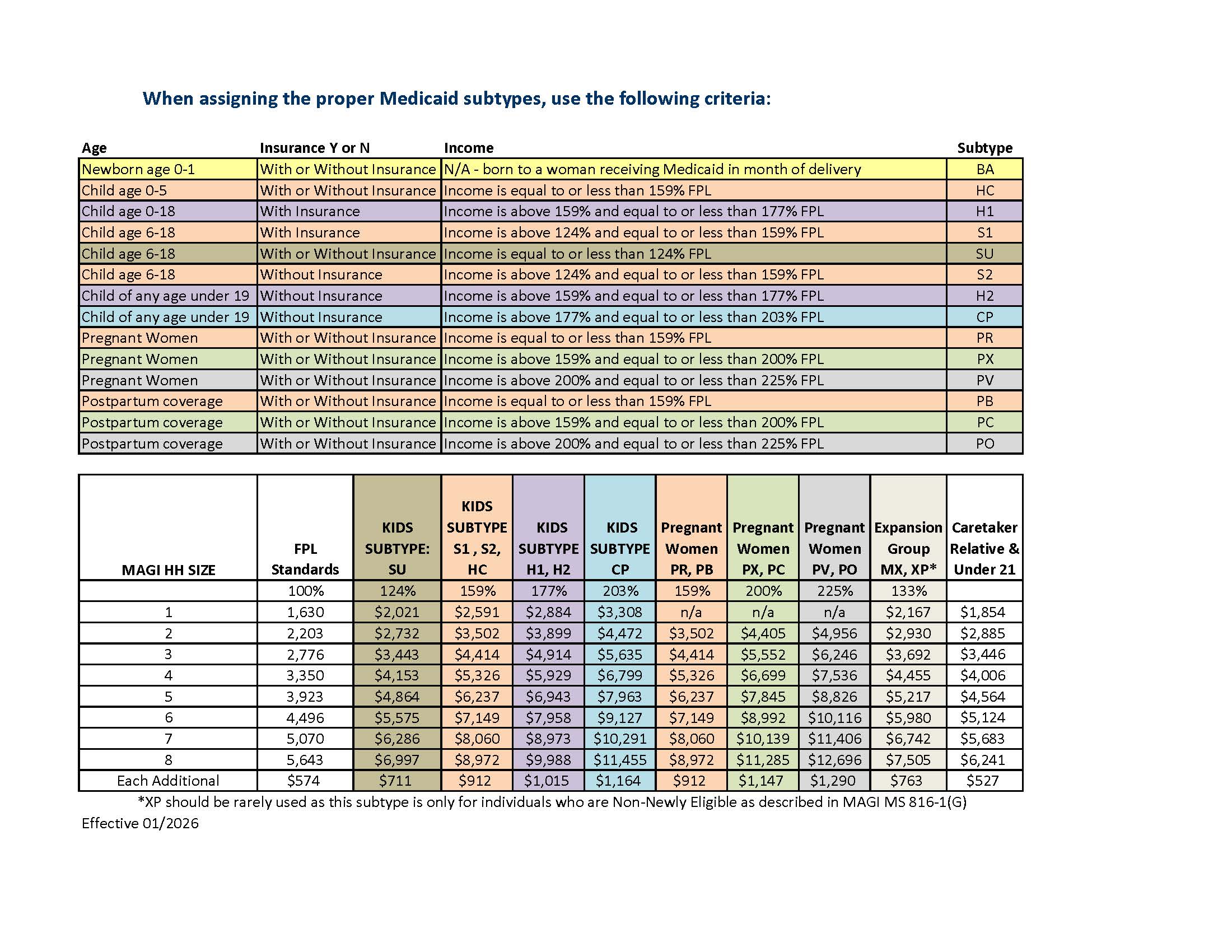
*XP should be rarely used as this subtype is only for individuals who are Non-Newly Eligible as described in MS 816-1(G).
|
|
||
|
|
|